Annual
Report

Christopher V. Goff, Esq.
Chairman, President & CEO
When reflecting on 2024, one word comes to mind: transformative. With the rapid growth of high-cost drug categories, the long-anticipated launch of Humira biosimilars, the expanding influence of state legislation and preparation for a new presidential administration, plan sponsors faced no shortage of change. Through it all, our team remains committed to helping plan sponsors nationwide make informed decisions, mitigate risk and deliver meaningful value and pharmacy solutions to their plan participants.
It was also a transformative year for Employers Health. In 2024, we experienced tremendous growth across our organization, allowing us to achieve major milestones. I am pleased to announce we welcomed 80 new clients and an additional $758 million in pharmacy spend, surpassing $4 billion in total. We now have clients in 42 states, covering more than 1.9 million lives in all 50 states. We're exceptionally proud of these milestones and eager to continue building on this momentum. Moreover, we expect 2025 to exceed 2024's results.
This incredible growth wouldn't be possible without our highly engaged clients, diligent consultants and talented team. As our team surpasses 100 dedicated colleagues consisting of pharmacists, account managers, analysts and legal professionals, the industry continues to evolve. We remain committed to delivering timely resources and the strategic services you have come to expect from Employers Health. As in previous years, state legislation was a dominant force in 2024. Our team monitored hundreds of proposals seeking to regulate pharmacy benefit managers (PBM) across all 50 states and, by extension, employer-sponsored group health plans. As many of these proposals aim to regulate employer plan sponsors subject to ERISA, we continued to educate legislators on the harmful impact these bills will have on plan sponsors. At Employers Health, we appreciate the effort that goes into the design and administration of affordable pharmacy benefits, and we're here to advocate on your behalf.
To further our commitment to helping employers maximize the value of their pharmacy benefits, we diligently evaluated additional PBM offerings. We are proud to share that we have added a third PBM option for 2025, MedImpact. An innovative PBM with high integrity, MedImpact offers clients more flexibility than other PBMs in designing their pharmacy benefit while maintaining competitive pricing guarantees. We are grateful for this new relationship and the outcomes and experiences it will bring for plans and participants.
As we look ahead, please know that the Employers Health team is here to improve your PBM experience. We thank you for your continued trust and support. Together, with our clients and their consultants, we look forward to achieving even greater success in the year ahead.

Mission
Employers Health is committed to providing resources, tools and expertise to help plan sponsors deliver high-quality health care benefits at a sustainable cost.
How we accomplish our mission:
- Managing group purchasing strategies
- Benchmarking and data interpretation
- Building physically and mentally healthy workforces
- Sharing ideas and best practices
- Collecting and analyzing market intelligence
- Supporting population health improvements
- Creating an environment where all team members bring their best selves

Vision
Employers Health is a premier, nationally recognized employer led organization focused on:
- Earning the trust of our clients and their consultants as a reliable and consistent resource for unbiased, objective resources and expertise
- Managing a variety of growing and market-leading collective purchasing solutions
- Achieving consistently high levels of client and participant satisfaction and loyalty by delivering on our promises and helping employers achieve their desired results

Value
Employers Health brings value through a host of solutions that help our clients achieve:
- Affordable, high-quality health care benefits
- Healthier employees who are more productive in their individual jobs, thereby creating better organizational performance
- An informed workforce that interacts with the health care delivery system more effectively, leading to better health outcomes and lower costs
- Fully engaged, resilient employees who can more effectively meet the challenges of today's work and family environments
- Work cultures with aligned incentives that produce employee loyalty and create "great places to work"
Reducing Rising Pharmacy Costs
Since 1995Employers Health has worked to reduce pharmacy benefit costs for plan sponsors for more than 30 years. Through the collective power of group purchasing for PBM services, plan sponsors maximize the value of their benefit plans while providing plan participants and their families with affordable pharmacy benefits. What started as a local initiative to contain pharmacy costs in Northeast Ohio has turned into one of the nation’s leading group purchasing organizations, covering more than 1.9 million lives. Today, more than 400 plan sponsors in 42 states benefit from these synergies created decades ago.
The Employers Health Difference
Since the beginning, we’ve been dedicated to providing the best PBM experience possible. Plan sponsors and their participants achieve value through better outcomes, better experiences and better costs, evidenced by the growth and retention of the Employers Health client base.
“Employers Health has provided me with unlimited resources in the pharmacy space so I can do a better job managing the company’s pharmacy spend while at the same time ensuring employees’ needs are met.”
– senior manager, benefits

Expert Resources
Employers Health clients stay up to date on industry and pharmacy trends crafted specifically for benefits professionals and written by our team of clinical and legal experts. Clients have exclusive access to a variety of helpful resources, including the Employers Health podcast, blog and webinars to use and share with colleagues.

Clinical Support
With a dedicated team of independent clinical pharmacists, clients receive ongoing clinical support from both the PBM and Employers Health. Our team of managed care pharmacists provide in-depth knowledge of PBM clinical capabilities, custom clinical programs, high-cost claim reviews and more.

Legal and Regulatory
The Employers Health legal team continuously monitors and reports legislative and regulatory developments and impacts directly to clients and their advisors. Our internal team works with the PBM to ensure adequate and timely compliance with reporting requirements and plan changes necessitated by state laws.
Better outcomes, better experiences, better costs
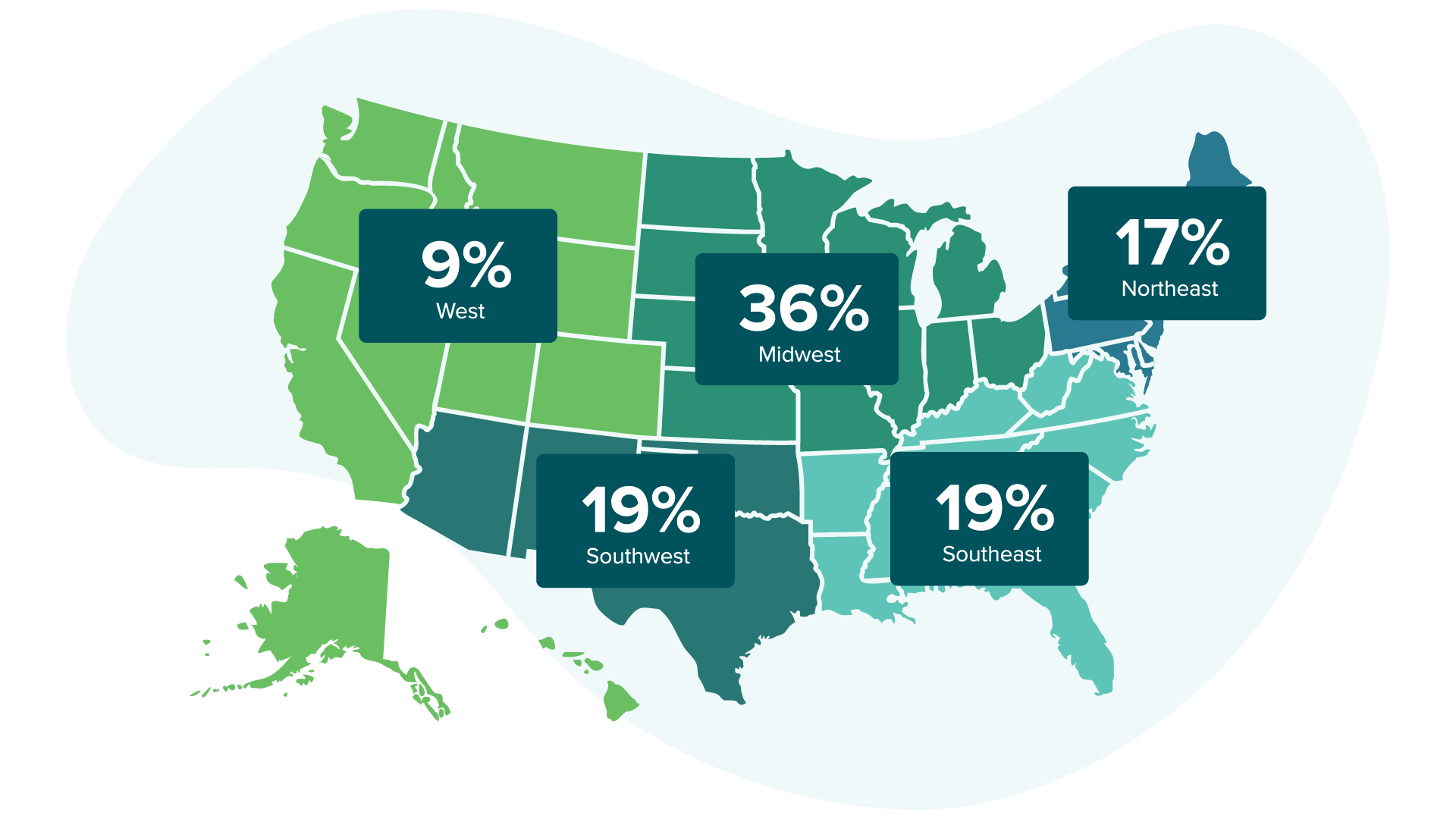
Clients By Region
Clients by Region
Clients by Industry
21%
manufacturing
22%
education and government
11%
health care
14%
financial and professional services
32%
other
80%
limit days’ supply on specialty drugs

96%
utilize the national retail network
97%
utilize the Advance Control Specialty Formulary
JANUARY 2013 RELATIONSHIP START
Optum Rx is a pharmacy care services company going beyond traditional pharmacy benefit management. With synchronized engagement, PreCheck MyScript and personalized care through Optum Specialty Pharmacy, Optum Rx provides customized solutions to employers.
Amongst Employers Health clients utilizing Optum Rx:

100%
limit days’ supply on specialty drugs

94%
utilize the exclusive specialty strategy

100%
limit new-to-market drugs
“The educational insights Employers Health brings to our annual pharmacy review meetings are unmatched.”
– benefits director
Clinical
As managing pharmacy spend becomes even more complicated, employers are seeking innovative ways to tackle the rising costs head-on. At Employers Health, our dedicated clinical team proactively monitors the pharmaceutical pipeline and analyzes our book of business. Their goal? To recommend and implement tailored clinical solutions that promote appropriate utilization and cost management of high-priced, low-value drugs. By staying one step ahead, we help employers achieve better adherence rates and consistently maintain flat-to-negative trend on targeted products.
Since 2016, our clinical team has identified over 1,000 unique drugs, multivitamins and combination products where custom clinical interventions could be implemented. These strategies primarily target medications that contribute to inefficient spending, focusing on strengthening the clinical criteria surrounding the appropriate use of costly drugs with a limited patient population. For the 2024 plan year, the team introduced and continued to tailor specific strategies for high-cost generics, obesity medications, acne treatments and sleep step therapy. By developing comprehensive reporting, they assess the savings achieved versus any potential disruption and offer valuable guidance to clients, ensuring the selected strategies align with their unique plan philosophy.
Beyond our custom management solutions, our clinical team provides value through:
- Weekly reviews of high-cost claims to check for clinical appropriateness
- Participation in client plan reviews
- Engaging blog posts and articles
- Expert presentations at conferences and webinars
The Employers Health clinical team is here as your resource for all of your clinical concerns.
Together, we can navigate the complex landscape of pharmacy costs and achieve optimal outcomes for your organization.
“The Employers Health team is experienced, very knowledgeable and responsive. They take the time to understand our organization and how it impacts our pharmacy decisions.”
– director, benefits planning
Client Solutions
The client solutions team at Employers Health is dedicated to enhancing results and achieving your goals, all while improving the participant experience. As a testament to their dedication to the industry, over half of Employers Health's client executives have obtained or are earning their Certified Employee Benefit Specialist (CEBS) designation through the International Foundation of Employee Benefit Plans. In addition, all client executives must complete their accident, health and life insurance licenses from the Ohio Department of Insurance.
We've constructed a team of benefits experts to help employers navigate the complexities of the pharmaceutical industry. Employers Health client executives serve as a conduit to the vast resources within Employers Health and your chosen PBM. Our size and scale allow us to take an active management approach in identifying proactive strategies for employers seeking to maintain a flat or negative trend in their drug spend. The team facilitates implementations, monitors spend and trend and delivers innovative solutions tailored to your population's unique needs.
In today's complex benefits environment, increasingly intricate knowledge is required of human resource professionals to manage the benefits offered to plan members effectively. PBMs are complex organizations that can be difficult to navigate without the assistance of an experienced professional. We strive to reduce or eliminate those complexities for our clients to create a better experience for the plan and its members. Our team seeks to aid our clients in the day-to-day management of the pharmacy plan, allowing them to direct their focus toward overarching benefits strategies.
Client Satisfaction Scores
Contract Management
Through comprehensive contract negotiations, clients participating in our pharmacy benefits group purchasing program have exclusive access to market-leading pricing guarantees, diverse network and formulary management options and robust service and performance guarantees.
One of the key components of the contractual arrangements between Employers Health and its PBM suppliers is the annual market check. The market check provision allows the Employers Health team to annually renegotiate the terms of its contractual arrangements to add service offerings, clarify terms, strengthen guarantees and, in a nutshell, adjust for market dynamics. Many PBM arrangements are three years long with no formal vehicle for adjustment based on market dynamics. Over a three-year period, significant changes occur in health care, and the PBM industry is no exception. An annual market check is critical to ensuring that Employers Health clients have a contract that stays abreast of current market dynamics.
The market check process integrates market intelligence and data analysis, with a significant portion of the market intelligence derived from participating in competitive bids. In 2024, Employers Health PBM contracts underwent over 300 evaluations, making them some of the most scrutinized contracts in the industry. Regardless of the result of these evaluations, the insights gleaned from our participation in the evaluation process help to identify areas of strength or weakness.
The challenge with intelligence from participation in competitive bids is that information gained from that process tends to be either too specific or broad. To get a complete picture of the strength of Employers Health's PBM offerings, each year Employers Health engages at least one national pharmacy practice to benchmark the aggregate value of the financial arrangements within its PBM contracts against rival offerings. Additionally, Employers Health leverages its data analytics and business intelligence teams to identify trends that will impact financial guarantees.

Ancillary Vendors

Quantum Health is the industry-leading consumer health care navigation and care coordination company that delivers an unparalleled consumer experience to its members, as well as validated claims savings and high satisfaction rates for its self-insured employer clients. Quantum Health's proprietary Real-Time Intercept® model identifies opportunities for early intervention in a member's health care journey, resulting in better engagement, outcomes and cost efficiencies.

EyeMed Vision Care is dedicated to helping members achieve better, healthier vision by giving them access to the right mix of independent eye doctors and national and regional retail providers so members can go where they want, when they want. EyeMed's client family is over 20,000 strong and covers nearly 78 million Americans in funded vision plans.

For over 40 years, ComPsych has developed and refined a comprehensive solution delivering the most holistic well-being experience in the market. As the worldwide leader in organizational mental health, resilience and absence management, we provide the industry's broadest range of people-centered, real-time and holistic solutions designed to help individuals thrive.
Smiles are important, and since dentists can detect more than 120 symptoms of non-dental diseases, it's essential to follow good oral health habits for better overall health. Delta Dental of Ohio began operations in 1960, and today with its affiliates, makes up one of the largest dental plan administrators in the nation.
“Employers Health has a team that goes above and beyond to help us accomplish our strategic priorities.”
– benefits manager
