As medical marijuana continues to gain approval at the state level, many questions arise regarding its safety and efficacy. Does scientific evidence support the use of medical marijuana? Should it be considered as a medication for certain disease states, and therefore, a covered benefit? This popular topic poses many challenges, including clinical, regulatory and ethical implications. In order to provide insight for employers, this article will highlight the pharmacology, therapeutic effects and conflicting evidence surrounding the use of medical marijuana.
Marijuana Background
The use of marijuana is associated with many common effects, such as relaxation, euphoria, increased sociability, hunger and altered sense of time. However, marijuana can produce other effects that may help to mitigate or treat symptoms associated with certain disease states. It can also exacerbate underlying conditions and produce undesirable side effects, such as paranoia and anxiety, particularly if the method of use and dosage is not considered, as is often the case.
Marijuana has multiple routes of administration with inhalation or smoking being the most commonly utilized. This route is also associated with the quickest onset of action and higher maximum concentrations within the blood compared to other routes. Advocates of medical marijuana believe that inhalation is a favorable route of administration because the user has some control over the dose they receive based on the depth of inhalation or puff rate. Other routes of administration include oral lozenges, gums, baked goods, beverages, sprays and topical products. The relationship between routes and proper dosage is very individualized and still not properly defined due to the lack of established evidence and guidelines.
Marijuana is prepared from various strains of the Cannabis plant. Specific parts of the plant produce greater amounts of active compounds. For example, the flowering tops and leaves secrete resin, which contains the active components that produce effects within the body. These active components are commonly referred to as cannabinoids. Although over 100 cannabinoids are known, the two most commonly known are delta-9-tetrahydrocannabinol (delta-9-THC) and delta-8-tetrahydrocannabinol (delta-8-THC). THC is the primary compound responsible for producing an altered mental sensation commonly referred to as the “buzz” associated with marijuana. Additionally, cannabidiol (CBD) is another well-known cannabinoid that produces non-psychoactive effects within the body. Therefore, it is thought that CBD can help relieve symptoms associated with a disease without producing the “buzz” sensation.
Pharmacology of CBD vs. THC
What produces these different effects between CBD and THC? When CBD and THC enter circulation, they mimic the naturally occurring cannabinoids in the body to act on cannabinoid receptors in order to produce both desired and unwanted effects. These cannabinoid receptors are in the brain as well as other organs throughout the body and make up the endocannabinoid system. Specifically, a receptor called CB1 is found throughout the central nervous system, which consists of the brain and spinal cord. Another receptor, called CB2, is present in cells and organs responsible for regulating immune functions as well as other functions.
THC can bind with CB1 receptors in the brain, which results in psychoactive effects, and the release of neurotransmitters. Neurotransmitters are chemical substances in the brain, such as dopamine, serotonin, norepinephrine, epinephrine and GABA. The exact mechanism of CBD is not completely understood, but research reports that CBD does not directly interact with the CB1 and CB2 receptors. CBD still results in an increase or decrease of neurotransmitters, but this occurs at a lesser extent compared to THC. These unique characteristics may contribute to its non-psychoactive properties and can even result in desired therapeutic effects. In fact, research reports that CBD shares many characteristics with anti-seizure medications and has anti-convulsant effects.
Approved Disease States
SUBSTANTIAL OR CONCLUSIVE EVIDENCE
Chronic Pain
Antiemetic
Patient-Reported Multiple
Sclerosis Spasticity Symptoms
MODERATE OR LIMITED EVIDENCE
Short Term Sleep Disturbance
Increasing Appetite
Decreasing Weight Loss
Clinician Measured Multiple Sclerosis Spasticity
Tourette Syndrome
Anxiety
Post-Traumatic Stress Disorder
Traumatic Brain Injury or Intracerebral Hemorrhage
INSUFFICIENT OR NO EVIDENCE
Cancer
Schizophrenia
Dystonia
Epilepsy
Irritable Bowel Syndrome
Amyotrophic Lateral Sclerosis
Huntington’s Chorea
Parkinson’s Disease or L-DOPA Induced Dyskinesia
Spasticity Due to Spinal Cord Injury
Since we are still in the infancy of marijuana research in the endocannabinoid system, there is currently no definitive answer regarding the exact conditions in which marijuana would be efficacious. A 2017 resource, “The Health Effects of Cannabis and Cannabinoids”, summarizes the conditions that have substantial or conclusive evidence for the use of medical marijuana. Researchers concluded that the strongest evidence currently supporting the use of medical marijuana is for three indications: 1) reduce nausea and vomiting associated with chemotherapy, 2) treat pain, and 3) relieve subjective spasticity in multiple sclerosis. Figure 1, is an excerpt from the “The Health Effects of Cannabis and Cannabinoids” and lists other conditions in which medical marijuana may help.
SUBSTANTIAL OR CONCLUSIVE EVIDENCE
Chronic Pain
Antiemetic
Patient-Reported Multiple
Sclerosis Spasticity Symptoms
MODERATE OR LIMITED EVIDENCE
Short Term Sleep Disturbance
Increasing Appetite
Decreasing Weight Loss
Clinician Measured Multiple Sclerosis Spasticity
Tourette Syndrome
Anxiety
Post-Traumatic Stress Disorder
Traumatic Brain Injury or Intracerebral Hemorrhage
INSUFFICIENT OR NO EVIDENCE
Cancer
Schizophrenia
Dystonia
Epilepsy
Irritable Bowel Syndrome
Amyotrophic Lateral Sclerosis
Huntington’s Chorea
Parkinson’s Disease or L-DOPA Induced Dyskinesia
Spasticity Due to Spinal Cord Injury
Marijuana vs. Opioids for Pain
As of August 2019, three states (New York, Illinois and Colorado) allow legal prescribing of medical marijuana for any condition instead of a prescription for an opioid. Although this alternative can be viewed as a strategy to help combat the opioid crisis, it does not come without concern. For example, this new law allows medical marijuana to be prescribed in place of an opioid, but other medications may be more clinically appropriate. Critics argue that a physician could theoretically bypass evidence-based guidelines for the specific condition and prescribe medical marijuana to help treat the associated pain. On the other hand, supporters argue that the law allows for open conversation between physicians and patients for the legal use of medical marijuana.
From a clinical perspective, there are additional considerations that need to be addressed regarding this law. If a patient is prescribed medical marijuana and was previously taking an opioid, he or she will need to be counseled to not use them concurrently. Medical marijuana can result in significant adverse effects, which may be more prevalent when used in combinations with prescription medications or in younger populations. Furthermore, there is conflicting evidence regarding the efficacy of medical marijuana. While pain is one indication for which medical marijuana has more conclusive evidence in the literature, individual studies have mixed results. However, a 2018 study in the Medicaid population showed states with medical cannabis laws saw roughly a 6% drop in opioid prescription rates. Perhaps more importantly, a 2014 study published in the Journal of the American Medical Association found that the average opioid overdose mortality rate was 24.8% less in medical marijuana states.
State Programs
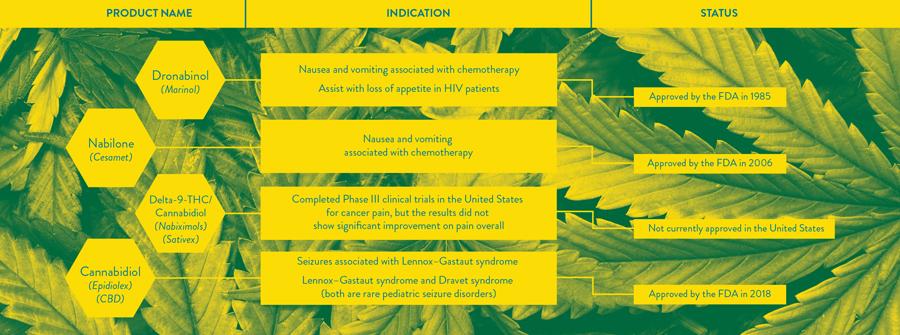
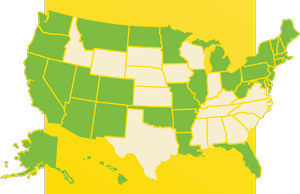
The illegality of marijuana traces its history to highly questionable tactics by Harry Anslinger as the U.S.’s first commissioner of the Federal Bureau of Narcotics, but it is still considered illegal at the federal level today. With the exception of the few products listed in Figure 2, marijuana is labeled as a Schedule I drug under the Controlled Substances Act, which means the DEA believes it has a high potential for abuse without any accepted medical benefit. This classification not only limits its ability for insurance coverage, but also research for therapeutic safety and efficacy as well. However, many states have enacted medical marijuana laws specific to each state. As of October 2018, 33 states have implemented such laws. Although each state’s law is different, most of the states permit the use of medical marijuana for the following conditions: cancer, AIDS/HIV, seizure disorders, specific types of pain and muscle spasms. Additional conditions may be approved depending on the state in which the patient resides. Other differences amongst states include: the amount of medical marijuana that can be purchased, the age of the patient, requirement for patient registration prior to use and residency requirements.
As new evidence emerges, medical marijuana will continue to raise questions and debates about coverage for employees outside of the workplace. It is worth noting that pharmacy benefit managers are not legally allowed to process claims for marijuana if it remains as a Schedule I drug by the DEA. Despite states permitting the use of medical marijuana for certain conditions, patients will still be responsible to cover the total cost and use will continue to be outside of medical records. Therefore, a patient’s health care team will have limited awareness of potential drug and disease state interactions.
It appears the only thing evident about medical marijuana is that further evidence is needed in order to provide definitive answers regarding the true impact of medical marijuana as a treatment regimen, the potential for benefit coverage and appropriate utilization management strategies. As the smoke clears on this budding topic, look for future updates from the Employers Health team.
Download Article