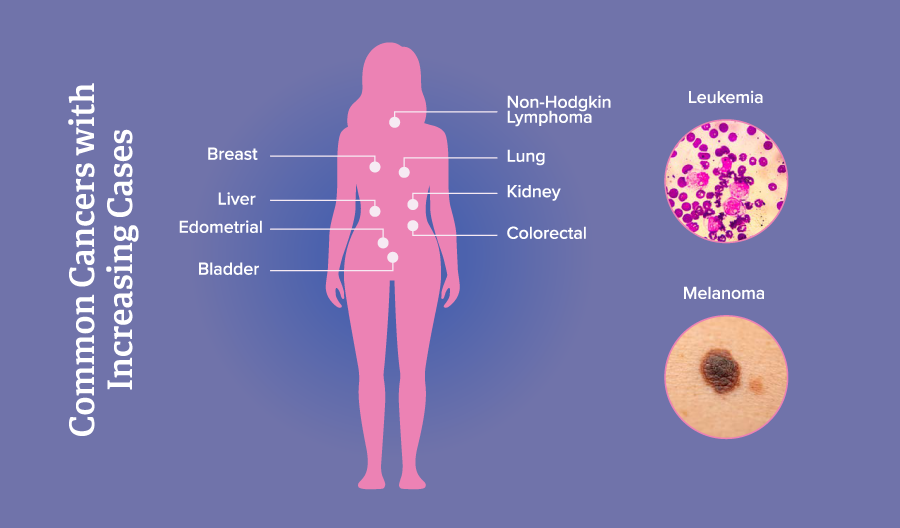
Did you know it’s predicted that six of the top 10 most common cancers (breast, prostate, melanoma, uterine corpus, pancreas and colorectal) in the 65 and under age group will see increases in cases throughout 2025?1 And, young women are nearly twice as likely to be diagnosed with cancer than young men. While cancer cases continue to rise, so do the costs of treatment and care, making up 6% of total health care spending in the U.S.2 With this growth comes greater threats to plan sponsor budgets and the need for more proactive measures to manage cancer holistically.
Within the Employers Health book of business, oncology is fifth in terms of net spend, costing approximately $13.71 per member per month (PMPM) as of Q4 2024. Along with diabetes, it is projected that oncology will be a top trend driver into 2028.3 Following a brief stall during the pandemic, there has been slow and steady growth year-over-year as patients returned to doctors for visits and screenings. Unfortunately, delays in these visits have led to diagnosis and progression to later stages of cancer, necessitating more expensive therapies.
Oncology management
From a management perspective, controlling cancer costs can be divided into two approaches: prevention and treatment. Oncology treatment and utilization management are typically handled very delicately under the pharmacy benefit. Oncology has historically been difficult to manage extensively. This is due to the high number of novel therapies, targeted mechanisms of cancer drugs and the sensitive nature of the disease state, where delays can negatively impact patient outcomes and disruption. At its most basic level, oncology agents should have a prior authorization (PA) that ensures the drug is being prescribed to label and adhering to National Comprehensive Cancer Society (NCCN) guidelines. Usually, this involves confirming that the patient is seeing the right type of specialist, undergoing the necessary lab tests and receiving appropriate support services. However, we have witnessed a maturation in the management landscape due to competition within treatment classes, generic launches and biosimilar development. Certain types of cancer such as breast and prostate now have multiple options to choose from which can help with pricing and formulary selection.
As median list prices of cancer treatments continue to rise, many employers are becoming more open to placing coverage restrictions on this class. One study found the use of restrictions for payers rose from 17.6% to 33.5% between 2017 and 2021.4 For example, the Employers Health clinical team launched a custom clinical PA for the prostate cancer drug, Yonsa (~$10,000 per Rx), which involves stepping through a generic for Zytiga called abiraterone (~$5,000 per Rx). While minimal differences were observed from a safety and efficacy perspective between Yonsa and abiraterone, a pathway of medical necessity was preserved to allow patients and providers to access Yonsa by providing appropriate clinical rationale. Regardless, the use of these traditional management methods remains limited, particularly for targeted and gene therapies. Instead, employers may find more value in holistic care and early prevention.
Cancer prevention best practices
Preventive measures involve promoting appropriate screenings and wellness visits to catch cancers early. As expected, early-stage diagnosis leads to better health outcomes and lower costs. While many employers provide free screenings and wellness visits, opportunities still exist to enhance employee communication and participation, target growing cancer areas and improve racial disparities within the system.
Employers Health recently collaborated with Genentech to provide plan sponsors with ideas to improve their plan design. Beyond incentivizing health care visits, recommendations include leveraging existing awareness weeks and months, providing additional reimbursement and time off for patients and even removing barriers to getting screened. Recommended cancer screening ages highlights the general age ranges provided by various cancer-focused institutes on when people should receive screening. In its approach to improving cancer care, Genentech removed age restrictions for cervical, colorectal, prostate screenings and mammograms. Additionally, it expanded coverage to include breast MRIs, ultrasounds, colonoscopy preparation kits and genomic testing to reduce patient cost.
While covering all these services and products may initially be a higher cost, these costs can often be offset through the early detection of cancer in plan participants. In a more targeted and financially conservative approach, plans do not necessarily have to turn on coverage for everything at once. Utilizing demographic health data can help employers identify high-risk populations to modify coverage in small but impactful ways.
Though a simple paragraph will not do this topic justice, it is important to talk about existing racial disparities in both prevention and follow-up treatment. While national trends may indicate one thing for the general populace, it is essential to understand that race and ethnicity are a significant factor in cancer. For instance, Black women have 40% higher mortality rates in breast cancer and two times higher rates in uterine corpus cancer despite similar incidence rates.4 This higher mortality rate in Black women can be partially attributed to the fact that Black women are less likely to receive a referral for a follow-up and mammogram after an abnormal result.1 These disparities are extensive and numerous and can range from medical factors like tumor biology, underlying diseases or diagnostic differences, to nonmedical social detriments like income and health care access and literacy. Employers need to be aware of this dynamic, so they may utilize demographic data to tailor plan designs to address these gaps.
Simply providing free screenings may not be adequate; comprehensive support is needed to ensure appropriate follow-up, access to high-quality institutions and health care navigation assistance. Fortunately, employers are not alone in finding ways to address these challenges. National initiatives, such as Cancer Moonshot and the Persistent Poverty Initiative, are working to provide the funding, research and resources necessary to foster change.5,6
So, what’s next?
The approach we outlined is crucial in addressing the many challenges posed by cancer in the workplace. The landscape of cancer management is evolving with drug development, rising incidence and demographic shifts influencing employer strategies. Prioritizing preventive measures and expanding how employers cover benefits to catch cancer early can support better health outcomes while reducing long-term costs. Employers Health provides our clients and consultants with resources and market updates to assist in decision-making regarding plan design beyond just pharmacy.
Download Article